What if we could simply wish away this annual annoyance? Think of it. More people would be apt to celebrate with double decker ice cream cones, sugar laden snack cake binges, and polar bear sporting events– with no threat of illness, why not? No need for the questionably effective flu shots, we could all do without the mercury anyway, right? We could be tempted to splurge just a little more in the frenzied year end sales events and venture out in the late-night crowds to grab that last minute gift– all with no thoughts of the dread “airborne” menace. Thus, to make a seemingly good scenario even better, our wintertime domestic economy would flourish!
Okay. Back to reality… As much as we may wish the above situation to be true, of all the assurances in life few are actually more certain than death, taxation, and, well, the return of seasonal influenza…
Estimates vary, but each year roughly 5-10% of the US population will get the “flu” and an estimated 200,000 will get so sick they have to be hospitalized (2). Then, just a short time after it makes its dread appearance, it vanishes clear out of sight! Why this sudden departure? Well, researchers have been asking this question for decades, and, incidentally, while they have not figured out exactly where the virus vacations, they do know the reason for it’s apparent disappearance– It has a lot to do with something called “absolute humidity.”
Absolute humidity, like the more commonly known term “relative humidity,” refers to the amount of moisture in the air– only that absolute humidity takes into account air temperature as well. Therefore, as a general rule, absolute humidity increases with increased temperatures. Why is this important? Well, because researchers have found that the lower the absolute humidity, the higher risk of contagious “aerosolized” influenza (3, 4).
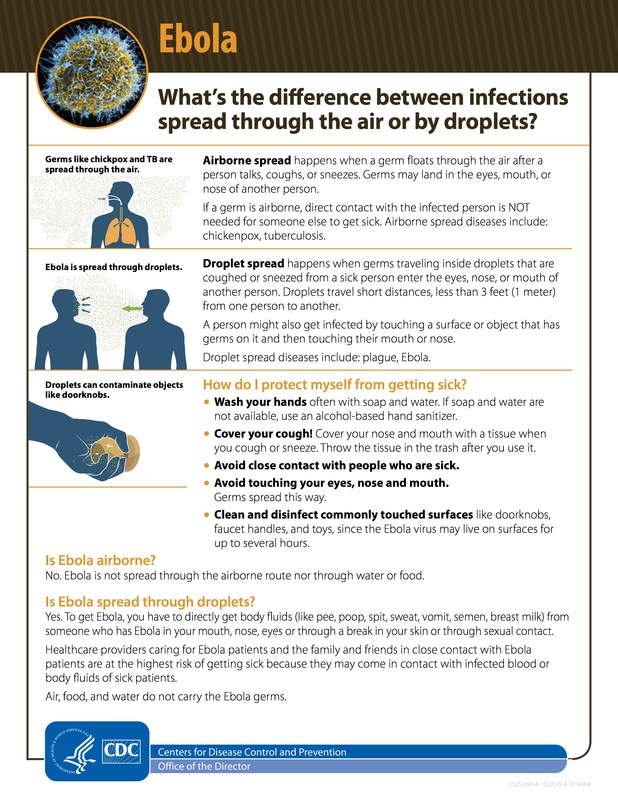
Before we go any further, let’s make sure we clear up any confusion regarding the definition of “aerosol.” Simply put, an aerosol is actually a combination of “airborne” and “droplets”. Airborne simply means that something is borne on the air. Scents, smells, and fragrances for instance are actually airborne particles that reach your sensory organs (olfactory bulb, etc.). However, a 747 jumbo jet is also “borne on the air.” The difference between the two is obvious- the 747 will quickly lose altitude because of its mass- a similar event occurs with very large droplets. What is a droplet? It’s actually a vague term used to describe an unspecified, but relatively small, quantity of liquid. It is possible for the human sneeze, cough, or breath to produce airborne droplets of various sizes: from a “few millimeters to less than 1 micro-meter in diameter” (5). How long these stay aloft, the distance they travel, and their infective potential will depend upon several factors: 1) their size; 2) force of expulsion; 3) and environmental conditions.
Now for the science behind the risk… Studies have found that “large droplets (>50 [micrometers] in diameter) settle on the ground almost immediately, and intermediate-sized droplets (10–50 [micrometers]) settle within several minutes.” “Small particles (<10 [micrometers]), including “droplet nuclei” from evaporated larger particles, can remain airborne for hours and are easily inhaled deep into the respiratory tract” (ibid). Since most viruses, including Influenza and Ebola (6), are less than 1 micrometer in diameter, they possess an inherent ability to be dispersed in aerosolized droplet form and, as the above definition states, “can remain airborne for hours and are easily inhaled deep into the respiratory tract” (ibid).
The frightening thing is that studies have revealed that as many as 87% -97% of particles in the breath can be of the smaller (< 10 micrometer) variety (7, 8). Traveling at tremendous velocities, up to 40 meters per second (9), the human sneeze, which contains up to 20,000 of these tiny droplets, is a significant aerosolization event! Comparatively speaking, although only several hundred droplets are usually produced by coughing (10), these potentially infectious particles are propelled at, an alarmingly fast, 100 meters per second (9)! Thus, given the fact that influenza grows so well in the upper respiratory system (in low absolute humidity environments), humans can become living “nebulizers”– scattering virus-laden droplets far and wide.
The good news is that, consequently, for certain viruses like influenza, rising absolute humidity occurring during the spring, summer, and fall significantly lessens infectivity. Therefore, during more humid conditions influenza is more readily transmitted by “close personal contact”– or through larger droplets of body fluid. Of note, researchers have cited the fact that it also takes an over two-hundred times larger dose of virus to cause an infection through this route, as compared to “airborne” inoculation (11, 3). Thus it becomes “harder to catch” - a term which sounds oddly familiar…
If influenza has a season is it possible that other viruses could operate in the same way? Could it be that other viruses that are “hard to catch” during the summer months, or, let’s say, in hot and humid sub-Saharan Africa, also spread like wildfire this winter? Let’s not postulate any longer. If you really want to know read on!
Is it possible that we have overlooked a potential threat that the domestically vanquished Ebola virus may return with a vengeance? Let's examine this possibility and "let the science lead us" to a logical conclusion...
First of all, studies have shown that, unlike what has been purported in the press, the Ebola virus itself has some degree of durability. It can be frozen, freeze-dried, exposed to varying pH changes, withstand substantial UV irradiation, and persist on certain mediums like plastic and glass for up to 46 to 50 days– all while still retaining the potential to cause illness (12, 13, 14). Also, contrary to what has been adamantly declared by public health officials, as one researcher put it “Filoviruses [such as Ebola] are relatively stable in aerosols” (ibid).
Furthermore, one article actually revealed the following: “human pathogenic filoviruses [like Ebola] may survive in an aerosol in the dark to detectable levels for at least 1.5 [hours]. If filoviruses were deliberately or accidentally aerosolized during normal laboratory or clinical practices they may pose a significant threat to humans, as they are able to remain infectious over a significant period of time” (13). Studies also reveal that “they [filoviruses] are highly infectious as respirable particles under laboratory conditions” (15) and “laboratory studies with monkeys demonstrate that the disease could potentially be transmitted through respirable [or inhalable] particles” (16).
If aerosolized Ebola virus is so dangerous, why then are the “experts” now so sure that Ebola does not spread via the air? For instance, months before the pandemic the Centers for Disease Control (CDC) reported that Ebola could be spread by aerosolized droplet (see figure A below). Why did they, after almost forty years of research and scientific evidence, suddenly change their stance?
I) It is reported that the typical route of current Ebola transmission is direct contact with Ebola-infected blood, body fluids, or large droplets.
II) Though numerous studies in animals have shown Ebola to infect lung tissue (17, 18, 19, 20), in humans it does not appear as though the lungs are a primary target of the virus (21, 22).
Let’s see how these arguments stand up to what has been previously reported in the scientific literature…
But first… a simple analogy: What if the CDC issued a statement that the “influenza virus is not spread via coughing, sneezing, or breathing?” Well, I believe that we would all wonder about the truth of such a claim. However, if the statement were issued during the summer months of heat and high absolute humidity, they would be correct. But, only until temperatures and humidity dropped again in the fall and the influenza virus became able to again thrive in the air. Ebola could have this same “seasonal” aerosol capability. Why? Because studies have shown that, unlike it’s native hot and humid African climate, Ebola is stable and infective at low absolute humidity (17).
Also, the fact that “we can’t believe it because we haven’t seen it” is also somewhat of a flawed argument. Given the magnitude of the current epidemic in sub-Saharan Africa and the fact that cases are underreported by a magnitude of up to 2.5 times (23), it is impossible to know how each infection occurred; and b) according to one study involving aerosol-based infection: “clinical signs” and “time to death” were “comparable” to infections caused by direct contact with infected blood or body fluids (24). Therefore, it is completely unreliable to base the “impossibility of aerosol transmission” upon the report of the patient or the apparent physical condition of the victim. That leaves only one argument left…
Can Ebola infect human lung tissue? To truly answer this question we to need examine Ebola “pathophysiology” or the way in which the disease operates… In humans, the Zaire Ebola virus seems to especially target the immune system and the liver (25). However, it is also documented that a lengthy Ebola infection can infect the cells that line blood vessels and the intestines, and then spread throughout the bloodstream reaching and infecting tissue in the vital organs (26, 27). The onslaught of the infection is so rapid, however, that most individuals die rather quickly from complications of the initial stages of infection: specifically from shock related to massive fluid loss caused by diarrhea, vomiting, and internal hemorrhage (21). Thus, in many cases, because of Ebola’s lethality, the infection may not significantly progress to the cells lining the airways– at least not enough to cause dramatic aerosol spread of the virus.
However, given the fact that the virus can reach high levels in the bloodstream and causes profuse internal bleeding throughout the body- including the lungs- (20), there is a very real danger of producing blood-tainted aerosolized respiratory droplets and secretions (28, 29, 30). This occurrence is, in particular, a major risk for healthcare workers caring for patients on ventilators. Furthermore, it is sufficient justification for the respiratory isolation of every Ebola patient. This is a sobering truth considering the fact that we have relatively few respiratory isolation units in modern hospitals. Thus, while we may be able to safely handle a few of these cases, we are definitely not ready for a pandemic scale event…
Another piece of the puzzle: in a strange and unexpected twist of logic, the widespread use of experimental medication, such “miracle drug” Zmapp, may be more of a hindrance than help. Why? It turns out that research scientists have found “that treatment [with monoclonal antibodies, and other experimental therapies] extended the time course of the disease and permitted the virus to infect tissues not usually affected in the typical model”…“in the brain, eye, pancreas, thyroid, and lung“ (31). Another similar study found that, although an experimental therapy may have helped a small percentage of monkeys to overcome the virus, these treatments lengthened the average fight against the fatal infection from 8 days to almost 13 days (32). Thus, by increasing the duration of the disease process, the virus has a much greater potential to reach higher levels in the lungs– a dangerous event highly favoring the airborne spread of the virus.
Thus we see that, indeed if we base our conclusions on the research, it is possible– even without further viral mutation (which is occurring at phenomenal rates)– to have an airborne-derived Ebola infection… With one stipulation, the infection will only occur under the “right” conditions. This would be in an environment with low absolute humidity, cooler temperatures, a victim that is being treated by experimental drugs, weakened immune systems, and, lastly, a population that does not believe it is possible to spread the virus through the air. Although we now meet much of the above criteria here in the United States, allow me to introduce Ebola’s highly probable “perfect storm…”
The Harmattan usually begins in late November and lasts until mid March (33). What is Harmattan? It describes a yearly phenomenon in which trade winds blow continually into western Africa from the Sahara desert– also marking the beginning of the dry season. These powerful gusts literally carry tons of mineral dust, much of which is actually blown across the Atlantic and settles in the Caribbean, Central America, and the southeast United States (34).
Furthermore, scientists have discovered that these giant dust clouds move tiny respirable (or inhalable) particles relatively quickly– reaching the southern United States in about seven days (ibid). Scientists have even postulated that viruses, especially after binding to dry desert mineral dust, in optimal climatic conditions (wintertime), may be moved from one continent to another through these winds (35, 36, 37, 38). Though many would think this scenario highly unlikely, consider the following researcher’s insight: “an entire city experiencing an epidemic could produce staggering amounts of virus aerosols, yielding something not unlike the medieval concept of infective miasma. It has been suggested that this mass of infective particles is responsible for the seasonality of influenza by using global convective currents” (35).
Interestingly, most US influenza outbreaks appear during Harmattan season and begin in the Caribbean and southeastern states (39). Could this be a coincidence? Although this is admittedly a source of debate, the Harmattan winds do, without a doubt, cause much harm in Sub-Saharan Africa.
Numerous studies document the fact that Harmattan season is also the time for western Africa’s yearly seasonal influenza pandemic. Researchers have found that “numerous studies of respiratory diseases, including those caused by influenza viruses, have suggested a closer correlation with the dry Harmattan season” (40, 41). These cases “increased at the onset of Harmattan” (42) and seem to peak around January (43, 44). This appears to line up with the finding that, during the Harmattan, temperatures and absolute humidity decrease from December through March – with coolest and driest period occurring in January (45).
As we have previously discussed, Influenza is not a major airborne threat unless these types of climatic changes occur. However, the Harmattan winds increase the potential for infection even further due to the inhalation of the dry airborne desert dust (11). Could this play a role in increasing Ebola risk? Well, one study revealed that inhaling high levels of particulate matter caused an inflammatory response in the lungs, which brought large numbers of white blood cells, and triggered the overproduction of the compounds tumor necrosis factor and nitric oxide (46, 47). These are same two chemical compounds is largely responsible for the Ebola’s hemorrhagic effects (48, 49). Thus, this increased lung inflammation would further raise the risk of infective aerosolized respiratory droplets.
Think this is bad? Just wait. There’s more to this risk than meets the eye. Seriously...
Because the Harmattan winds are a disruption of normal trade winds and pass through arid desert landscapes, the air molecules lose their vitality or electrical charge. This process is referred to as “positive ionization” and has disastrous consequences upon physical and mental health. For the sake of brevity, we will only focus upon two aspects: viral illness and mental stability.
Studies have shown that influenza infected mice exposed to positively ionized air had accelerated infections and greatly increased mortality rates (50, 51). Furthermore, exposure to atmospheric positive ions has been documented to increase the productions of stress hormones– notably norepinephrine– even to a “state of exhaustion” after several days (52). Researchers have found that high levels of norepinephrine suppress the innate immune response (53), which is a critical component in the fight against Ebola (54).
Increased stress hormones and a disruption of the normal breakdown of a neurotransmitter, known as serotonin, also cause significant mental disturbances. These include irritability, increased suspicion, aggression, and even criminal behavior– not a good combination with the law and order necessary to curtail this pandemic (55, 56). To make matters worse, disruption of the normal breakdown of serotonin can correlate into lower melatonin levels, the nighttime “healing hormone”, which can further depress innate immune system function (35).
If you think all of these factors are reason for concern we have not even mentioned the fact that the Harmattan causes widespread temperature fluctuations (57)– which have been shown to potentially increase all-cause mortality rates by up to 50% depending on geographic location (58). And, another yet unmentioned factor is that these dry desert winds increase the likelihood of dehydration: which just happens to be one of the most lethal complications of Ebola infection (59, 60, 61). The dry skin, dry mucous membranes, frequent nosebleeds, and chapped bleeding lips experienced by West Africans during this season all increase risk for disease spread (62).
And now– the ultimate danger… This danger is not as significant of a threat in Sub-Saharan Africa… but indeed much closer to home…
A strange phenomenon occurs when a population is warned of an occurrence that does not immediately appear– known officially as the “cry-wolf” effect. As the US has now been “officially cleared” from Ebola infection, have we relaxed our vigilance? Seeing that an optimally functioning immune system easily defeats Ebola (63, 64, 27), are we advising our population as to the need to engage in health promotion activities? Considering the fact that our healthcare system is decades behind in this area– with little focus and expenditure on population-based public health promotion (65, 66)– wouldn’t it be wise to take this pandemic threat as a wake-up call? Yes, we know things are still bad in Africa, but who is still sounding the warning back here at home? Or, are we still looking at the handful of cases we have successfully “treated” here in the US as evidence that there is really no threat from Ebola after all…
With flu season right around the corner the CDC has issued a startling acknowledgement that: "it is usually not possible to determine whether a patient has seasonal influenza or Ebola infection based on symptoms alone" (67). Thus, new Ebola cases have a high likelihood of being mistaken and treated as seasonal influenza– making conditions rife for an unpredictable outbreak... Meanwhile, when new potential Ebola cases arise, health officials are assuring the public that they are "perfectly safe" and that "fear is not going to help you make good decisions"– exactly the same message that greatly increased the casualties from the last major worldwide viral pandemic in 1918 (68, 69). When will we learn from our mistakes?
As one research scientist put it “the consequences of failure to warn can be serious for society overall, for example, significant economic losses, heavy infrastructure and environmental damage, large number of human casualties, and social disruption” (70). Are we ready to face such consequences?
Now is the time to prepare– but most of us have been lulled into a potentially fatal apathy…
References:
1) http://www.cdc.gov/flu/about/season/flu-season-2014-2015.htm
2) http://www.cdc.gov/flu/about/qa/disease.htm
3) http://wwwnc.cdc.gov/eid/article/12/11/pdfs/06-0426.pdf
4) Proc Natl Acad Sci U S A. 2009 Mar 3;106(9):3243-8. doi: 10.1073/pnas.0806852106. Epub 2009 Feb 9.
5) Adv Virol. 2014;2014:859090. doi: 10.1155/2014/859090. Epub 2014 Aug 13.
6) http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/ebola-eng.php
7) BMC Pulm Med. 2012 Mar 21;12:11. doi: 10.1186/1471-2466-12-11.
8) PLoS One. 2008 Jul 16;3(7):e2691. doi: 10.1371/journal.pone.0002691.
9) J Hyg (Lond). 1946 Sep;44(6):471-9.
10) http://www.influenzareport.com/ir/pathogen.htm
11) Environ Int. 2013 Sep;59:384-8. doi: 10.1016/j.envint.2013.06.022. Epub 2013 Aug 1.
12) Vopr Virusol. 1995 Mar-Apr;40(2):74-6.
13) J Appl Microbiol. 2010 Nov;109(5):1531-9. doi: 10.1111/j.1365-2672.2010.04778.x. Epub 2010 Jun 10.
14) Viruses. 2012 Oct 15;4(10):2115-36. doi: 10.3390/v4102115.
15) Biosecur Bioterror. 2004;2(3):186-91.
16) Appl Environ Microbiol. 2008 Feb;74(3):555-63. Epub 2007 Dec 7.
17) Int J Exp Pathol. 1995 Aug;76(4):227-36.
18) J Infect Dis. 2011 Jul 15;204(2):200-8. doi: 10.1093/infdis/jir077. Epub 2011 May 12.
19) Sci Rep. 2012;2:811. doi: 10.1038/srep00811. Epub 2012 Nov 15.
20) J Pathol. 1985 Nov;147(3):199-209.
21) Pol Merkur Lekarski. 2003 Feb;14(80):146-9.
22) N Engl J Med. 2014 Nov 5. [Epub ahead of print]
23) http://www.cdc.gov/mmwr/preview/mmwrhtml/su6303a1.htm?s_cid=su6303a1_w
24) Microbes Infect. 2011 Oct;13(11):930-6. doi: 10.1016/j.micinf.2011.05.002. Epub 2011 May 25.
25) J Infect Dis. 2011 Nov;204 Suppl 3:S957-67. doi: 10.1093/infdis/jir326.
26) Virology. 2007 Jul 20;364(1):45-54. Epub 2007 Mar 27.
27) Nat Med. 1999 Apr;5(4):423-6.
28) Ann Am Thorac Soc. 2014 Nov;11(9):1341-1350.
29) http://www.purdue.edu/newsroom/releases/2014/Q3/purdue-expert-showed-ebola-can-enter-cells-that-line-the-trachea-and-lungs-says-airborne-transmission-is-not-an-impossibility.html
30) J Virol. 2003 May;77(10):5902-10.
31) J Infect Dis. 2007 Nov 15;196 Suppl 2:S323-8.
32) J Infect Dis. 2007 Nov 15;196 Suppl 2:S390-9.
33) http://www.britannica.com/EBchecked/topic/255457/harmattan
34) Proc Natl Acad Sci U S A. 1999 Mar 30;96(7):3396-403.
35) J Virol. 2007 Jun;81(11):5429-36. Epub 2006 Dec 20.
36) Arch Environ Health. 2003 Aug;58(8):498-504
37) Microb Ecol. 2012 Nov;64(4):973-85. doi: 10.1007/s00248-012-0088-9. Epub 2012 Jul 4.
38) Rev Infect Dis. 1989 May-Jun;11(3):494-7.
39) http://gis.cdc.gov/grasp/fluview/main.html
40) J Infect Dis. 2012 Dec 15;206 Suppl 1:S121-8. doi: 10.1093/infdis/jis584.
41) http://af.reuters.com/article/topNews/idAFJOE81706Z20120208
42) Health Place. 2014 Jan;25:47-55. doi: 10.1016/j.healthplace.2013.09.009. Epub 2013 Oct 21.
43) BMC Public Health. 2014 Sep 20;14:981. doi: 10.1186/1471-2458-14-981.
44) Influenza Other Respir Viruses. 2014 Sep;8(5):524-9. doi: 10.1111/irv.12259. Epub 2014 Jul 29
45) Abdulhamid G. 2011. Relationship between some meteorological parameters in Ilorin, North Central Nigeria. Comp. Eng. Intell. Sys. 2: 46–52
46) J Toxicol Environ Health A. 2002 Oct 25;65(20):1571-95.
47) J Toxicol Environ Health A. 2002 Oct 25;65(20):1597-613.
48) J Virol. 2005 Aug;79(16):10442-50.
49) J Virol. 2004 Oct;78(19):10370-7.
50) Int J Biometeorol. 1970 Sep;14(3):247-60.
51) Science. 1976 Sep 24;193(4259):1209-13.
52) Zentralbl Bakteriol Mikrobiol Hyg B. 1982 Apr;176(1):72-8.
53) Proc Natl Acad Sci U S A. 2014 May 20;111(20):7379-84. doi: 10.1073/pnas.1322174111. Epub 2014 May 5.
54) J Exp Med. 2004 Jul 19;200(2):169-79. Epub 2004 Jul 12.
55) Science. 1976 Sep 24;193(4259):1209-13.
56) Fortschr Med. 1977 Mar 17;95(11):746-52.
57) J Equine Sci. 2014;25(1):1-6. doi: 10.1294/jes.25.1. Epub 2014 Apr 22.
58) Kalkstein, L.S., and R.E. Davis, 1985: The development of a weather/mortality model for environmental impact assessment. Proceedings of the 7th Conference of Biometeorology and Aerobiology, 334-336.
59) N Engl J Med. 2014 Nov 12. [Epub ahead of print]
60) Am J Respir Crit Care Med. 2014 Oct 1;190(7):733-7. doi: 10.1164/rccm.201408-1514CP.
61) Ann Am Thorac Soc. 2014 Nov 4. [Epub ahead of print]
62) Eur J Epidemiol. 1997 Oct;13(7):807-15.
63) Lancet. 2000 Jun 24;355(9222):2210-5.
64) Clin Exp Immunol. 2001 Jun;124(3):453-60.
65) https://archive.org/details/forhealthynation00unse
66) http://www.healthislife.org/why-healthislifeorg.html
67) http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/qa.html
68) http://www.boston.com/news/local/massachusetts/2014/12/02/suspected-ebola-patient-being-treated-boston-hospital/kjQngynamiuqmmLOi3lrVN/story.html
69) http://www.healthislife.org/health-news/ebola-can-you-handle-the-truth
70) Am J Disaster Med. 2013 Autumn;8(4):243-52. doi: 10.5055/ajdm.2013.0130.

 RSS Feed
RSS Feed